Explanation:
The most significant and clinically significant degree of the block is typically a complete block. Additionally, it is the block most likely to result in cardiovascular collapse.
Explanation:
TCP is substituted by the infusions of epinephrine and dopamine. An IV push drug called atropine is used to raise the heart rate.
Explanation:
Bradyarrhythmia refers to any rhythm problem with a heart rate less than 60 beats per minute. Keep in mind that a patient's symptoms are typically brought on by bradycardia when the rate is fewer than 50 beats per minute.
Explanation:
When these three conditions are met, clinically speaking, bradycardia with symptoms exists.
Explanation:
All of these signs and symptoms stem from a reduction in perfusion brought on by a sluggish heartbeat.
Explanation:
Both of the aforementioned symptoms are considered indicators of symptomatic bradycardia.
Explanation:
The main criterion for deciding whether to utilize the bradycardia algorithm is adequate perfusion.
Advertisement
Explanation:
ACLS Provider Manual for AHA, P. 73 The dose at which consistent capture is observed should be 2 mA above the current milliaperes output. Depending on the type of monitor you are using for your defibrillator, the aforementioned capture setting may change.
Explanation:
Page 73 of the AHA ACLS Provider Manual, box near the bottom of the page Set the demand rate to 60/min. Once pacing capture has been attained, this can be changed upward or downward.
Explanation:
P. 73 of the AHA ACLS Provider Manual It is not recommended to check the carotid pulse for mechanical capture. Muscle jerks brought on by electrical stimulation may resemble the carotid pulse.
Explanation:
All of the rhythms indicated in AHA ACLS Provider Manual P. 74 can quickly deteriorate into more dangerous conditions and signal the need for immediate transcutaneous pacing.
Explanation:
P. 69 of the AHA ACLS Provider Manual A chronotropic medication infusion to stimulate the heart is an alternative to pacing if symptomatic bradycardia is resistant to atropine. Start administering epinephrine at 2–10 mcg/min and titrate based on the patient's response.
Explanation:
P. 72 of the AHA ACLS Provider Manual A temporary intravenous pacemaker is inserted during transvenous pacing. TCP is less efficient than transvenous pacemakers since electrical impedance is essentially reduced. The wire in the vein(s) carrying the electrical current travels to the heart's pacing electrode.
Explanation:
When the impulse produced in the SA node of the atrium does not reach the ventricles and there is no discernible connection between P waves and QRS complexes, a third degree AV block, also known as a full heart block, develops.
Advertisement
Explanation:
P. 66 of the AHA ACLS Provider Manual
1 degree block = PR prolongation
Wenckebach = Mobitz I = 2nd degree block type 1
Hay = Mobitz II = 2nd degree block type 2
3rd degree block = complete block
Explanation:
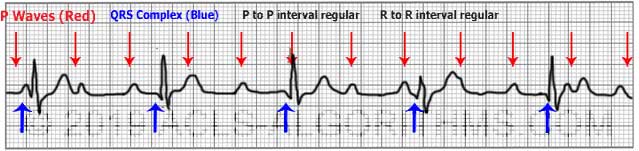
The AHA ACLS Provider Manual, page 67 On page 67, you may see a list of all the main bradycardia rhythms you'll come across. This rhythm strip is regular, has a constant and typical PR interval, and has a somewhat slower tempo than usual.