NREMT Practice Test
You are assessing the vital signs of a child at a public health center. Which of the following would be considered a normal set of vitals for a healthy nine-year-old child?
Correct answer: Respirations 20 breaths per minute, heart rate 98 beats per minute, BP 106/78 mmHg.
Vital signs in children need to be carefully interpreted within the overall history, context of appearance, work of breathing, and circulation to the skin (the Pediatric Assessment Triangle) and the entire physical assessment.
Normal values vary with age, and more important than identifying ""normal"" signs in a pediatric patient is to be aware of indications of respiratory distress/failure and circulatory shock. Serial assessments showing a trend over time may be more accurate and more useful.
Pay attention to extremes. Bradycardia indicates critical hypoxia or ischemia. Rapid respiratory rate of >60 breath/min (any age) or <20 bpm (children under 6), or <12 bpm (older children) are considered red flags. A ""normal"" respiratory rate alone never guarantees adequate oxygenation or ventilation.
Blood pressure may be difficult to assess in children, because of lack of cooperation, confusion about cuff size, and remembering normal values for a specific age. And a normal blood pressure may be misleading. Hypertension is not a clinical problem for children in the field. A low blood pressure definitely indicates hypotensive shock, and a ""normal"" value may be compensated shock.
Vital Signs per Age
Age, Respiratory Rate (breaths/min), Heart Rate(beats/min), Minimum Systolic BP(mmHg)
Infant (birth to 12 mo), 30-60, 100-160, >60
Toddler (1-3 yr), 24-40, 95-150, > 70
Preschooler (4-5 yr), 22-34, 80-140, >75
School-age child (6-12 yr) 18-30, 70-120, > 80
Adolescent (post-puberty) 12-16, 60-100, > 90
A patient who is unresponsive is discovered wet in a bath tub. She is apneic and has no pulse. What is the best course of action to take first?
Correct answer: Begin CPR while moving the patient out of the rain in anticipation of defibrillation via an automatic external defibrillator (AED).
Any patient who is without a pulse should receive CPR. While early defibrillation is critical, CPR should not be withheld or delayed. When a patient is unresponsive and has no pulse, an AED should be used. If a patient is unconscious, an AED should not be utilized.
If an ALS service is not available, which of the following is not a common rule for transporting a cardiac arrest patient?
Correct answer : All cardiac arrest patients must be sent right away.
Local protocol should be respected at all times. However, the following are general principles for transporting a cardiac patient during resuscitation/defibrillation efforts: if there is a return of spontaneous circulation (ROSC); if six to nine shocks have been provided and the patient is still in cardiac arrest; and if the AED sends out three successive “no shock advised” notifications.
In most cases, which of the following is not included in a patient care report?
Correct answer: Immunization record.
The following are generally included on a patient care report:
patient information and demographics
chief complaint
level of consciousness
vital signs
objective and subjective findings on assessments
treatment provided
times of incident reporting, EMS notification, EMS arrival on scene, EMS departure from scene, EMS arrival at receiving facility, and transfer of patient care
A six-year-old is unable to communicate. The carotid pulse is measured at 64 beats per minute and is judged to be normal. Breaths are shallow and come in at a pace of six per minute. Which of the following is the best course of action?
Correct answer: Begin the assisted ventilation process.
Respiratory arrest is the most common cause of cardiac arrest in children.
A patient who is not adequately breathing and has a palpable pulse should be provided assisted ventilation; the rate of ventilation for a child is one breath every three to five seconds (twelve to twenty breaths per minute). Children in this scenario should be placed in a position that allows for the management of the airway.
An adult patient with a palpable pulse should not be given chest compressions; CPR should be initiated on a child without a palpable pulse or a pulse less than 60 beats per minute.
High-flow oxygen would not be appropriate for a patient who is not breathing adequately.
The diastolic blood pressure is best described by which of the following statements?
Correct answer: During the relaxation phase of the ventricles, residual pressure remains in the arteries.
Blood pressure is separated into two components: systolic pressure and diastolic pressure. Systolic pressure is the pressure within the artery that occurs with each contraction of the ventricle and the pulse wave that it produces. Diastolic pressure is the remaining pressure during relaxation of the ventricles.
Snoring respirations are heard during the initial assessment of a semiconscious patient's airway. What are these breathing patterns indicating?
Correct answer: A partially obstructed airway
Snoring is an indication that the upper airway is partially obstructed.
Fluid or secretion in the upper airway will manifest as gurgling, which requires suctioning. If the bronchi are constricted, wheezing will be heard. This commonly occurs in asthmatic and chronic obstructive pulmonary disease patients. Crackles (formerly rales) are the sounds of air trying to pass through fluid in the alveoli. Crackles are a result of congestive heart failure or pulmonary edema.
During the inhalation phase of ventilation, which of the following occurs?
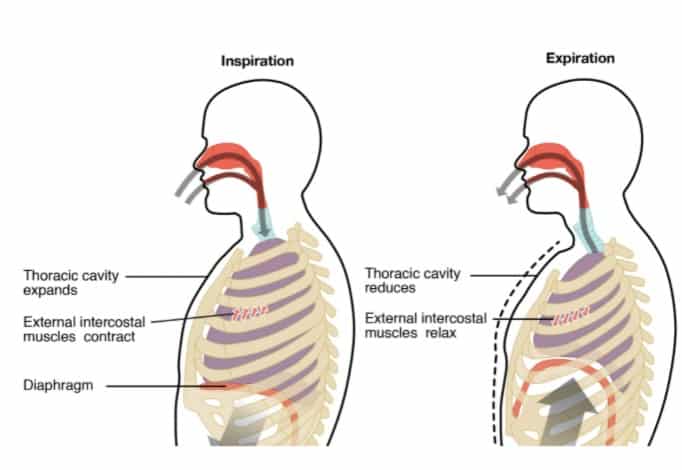
Correct answer: A partially obstructed airway.
Snoring is an indication that the upper airway is partially obstructed.
Fluid or secretion in the upper airway will manifest as gurgling, which requires suctioning. If the bronchi are constricted, wheezing will be heard. This commonly occurs in asthmatic and chronic obstructive pulmonary disease patients. Crackles (formerly rales) are the sounds of air trying to pass through fluid in the alveoli. Crackles are a result of congestive heart failure or pulmonary edema.
A 30-year-old man has been injured after falling from a two-story ladder. He is conscious and guarding his right thigh while bleeding from a wound on his left forearm. What is the most appropriate next step after completing a scene size-up and creating an overall impression?
Correct answer: Assess the airway of the patient and stabilize the C-spine.
After completing scene size-up, forming a general impression and assessing the level of consciousness, the airway of the patient is the first priority. Management of circulation issues (e.g., bleeding from the left forearm) is completed after assessment and treatment of life-threatening airway and breathing issues. The right thigh will be assessed during a rapid exam and then again during a secondary assessment. In cases of life-threatening bleeding, controlling bleeding takes priority over airway and breathing concerns.
An oropharyngeal airway is contraindicated in a conscious patient.
A patient with a cardiac history is experiencing chest pain. Which of the following is not a common symptom or sign linked with cardiac insufficiency?
Correct answer: Significant numbness or tingling on one side of the body.
Acute coronary syndrome (ACS) is a group of symptoms caused by myocardial ischemia; the most notable symptom is chest pain that is described as pressure, heaviness, or ""crushing."" It should be noted that not all patients have chest pain during ACS or an acute myocardial infarction (AMI). Additional signs and symptoms of ACS/AMI include weakness, syncope, dyspnea, nausea/vomiting, and pain that radiates to the lower jaw, neck, arm, or abdomen; other signs/symptoms include diaphoresis, pulmonary edema (pink frothy sputum), and irregular cardiac rhythm. Any patient complaining of nontraumatic chest pain should be assumed to have an AMI until that is ruled out by a physician.
Weakness, numbness, and tingling on one side of the body are more typically associated with a cerebrovascular accident (stroke).
A patient's generalized motor seizure has now come to an end. The patient is most likely to be in which of the following states?
Correct answer: Self-resolved lack of orientation to person, place and time.
After a seizure has ceased, a patient will be in a postictal state. An altered mental status is common; muscles relax, becoming almost flaccid or floppy, and breathing is labored to compensate for acidosis. Patients may also have hemiparesis, weakness on one side of the body.
Full orientation or anxiety/restlessness is not commonly seen in patients after a seizure. Alternatively, a patient will likely be responsive to painful stimuli, but, as above, be confused and lack orientation.
After swimming in a cold river, a 35-year-old man has developed hypothermia. Despite the fact that he emerged from the river in a matter of minutes, he seemed to be suffering from a loss of consciousness. Which of the following is the best course of action?
Correct answer: Cover the patient with blankets and turn up the heat in the ambulance's patient compartment.
Passive rewarming is an appropriate first step when dealing with a patient who has mild hypothermia. Passive rewarming includes placing the patient in a warm environment (e.g., the patient compartment with the heat turned up), removing wet clothing, applying heat packs/hot water bottles to the groin, axillary, and cervical regions, placing dry blankets over and under the patient, and giving warm, humidified oxygen.
Heat packs/hot water bottles should not be applied directly to the skin, to avoid burns.
Stimulants such as coffee, tea, soda, or tobacco products should be avoided, as they are vasoconstrictors which may further impair circulation.
Patients should be discouraged from walking, in order to not further damage the feet.
Massaging the extremities or handling the patient roughly is inappropriate.
In a patient with suspected cardiac chest discomfort, which of the following is a contraindication to nitroglycerin administration?
Correct answer: The systolic blood pressure of the patient is less than 100 mmHg.
Nitroglycerin is a vasodilator that is indicated for patients with cardiac chest pain. Acute coronary syndrome can present with chest pain/discomfort that is typically described as pressure or heaviness, nausea/vomiting, and sweating. Medical direction must be contacted and the “six rights” must be checked before administration of this medication.
Nitroglycerin is contraindicated in patients who have a systolic blood pressure of less than 100 mmHg, patients with a head injury, patients who have taken erectile dysfunction medications within the previous 48 hours, and patients who have already taken their maximum dose (typically three doses).
Most patients are allowed to repeat doses (typically up to three) if pain remains after five minutes; because of the previously mentioned contraindication, blood pressure should be assessed before administration of initial or repeat nitroglycerin.
In the prehospital situation, which of the following is not considered common personal protective equipment (PPE)?




Correct answer: Bulletproof vest.
Gloves, masks, respirators, barrier devices, and gowns are all regularly used personal protective equipment (PPE) in the prehospital setting. Each scenario may dictate a varied level of required PPE. Standard precautions should always be applied.
Body armor (bulletproof vest) is generally not part of everyday PPE. Some areas may require body armor; however, policy for most departments directs EMS personnel to avoid situations in which gun violence occurs.
A complication of poor hand placement during chest compressions is which of the following?
Correct answer: Fractured ribs.
When performing chest compressions during CPR, proper hand position and technique are important. In an adult, the heel of one hand should be placed on the lower half of the sternum, with the other hand placed on top of the first. Chest compressions should be done in cycles of 30 followed by two assisted ventilations. Compressions should be at a depth of 2 to 2.4 inches (5 to 6 cm) and at a rate of 100 to 120 per minute. If compressions are not done correctly, adequate circulation and perfusion will not occur. Potential complications of compressions can include fractured ribs or sternum and a lacerated liver.
Fractured clavicles, gastric distension, and a lacerated spleen are not likely complications of chest compressions.
Given the scenario, which of the following is a suitable intervention during triage of a mass-casualty incident?
Correct answer: Opening the airway of an unconscious patient with a pulse.
Simple assessment and correction of life-threatening conditions may be completed during triage (e.g., opening the airway, control of severe bleeding).
Environmental conditions and fractures are not treated during triage, but may affect the priority of a patient.
A pulseless patient is considered expectant (black tag) during a mass casualty incident; these patients are given the lowest priority, as they are not likely to survive.