FREE ABIM MCQ Questions and Answers
A 32-year-old female non-smoker appears with a few months' worth of exertion-related dyspnea.
She has experienced a spontaneous pneumothorax in the past. A typical CT picture is displayed. Which diagnosis is more likely?
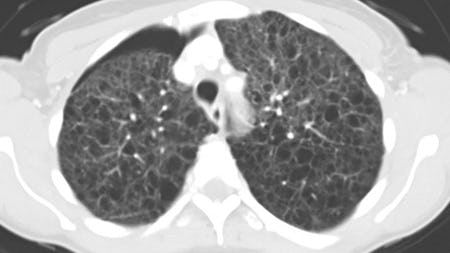
Pulmonary lymphangioleiomyomatosis (LAM) is a rare lung disease characterized pathologically by cyst formation and multifocal, nodular proliferation of immature smooth muscle and perivascular epithelioid cells (LAM cells). High-resolution CT scans show characteristic diffuse thin-walled cysts. In a relatively young female non-smoker of child-bearing age, this is the most likely diagnosis. Most patients are symptomatic at presentation, with dyspnea being the most common complaint. Complications include pneumothorax, hemoptysis, chylothorax, chyloperitoneum, chylopericardium, and development of lymphangioleiomyomas of the lymph vessels.
An occasional burning sensation in the lower extremities has been prevalent in the patient for the past 50 years.
The patient routinely exercises and follows a strict vegan diet. The previous medical history is not noteworthy. The physical examination went as expected. The results of pertinent tests are displayed below. Which of the following best represents the evaluation's next phase?
Clinical signs of vitamin B12 insufficiency in this patient include macrocytic anemia, neurological symptoms, a strict vegan diet, and borderline blood B12 levels. Methylmalonic acid and homocysteine levels can be checked in this situation to confirm the diagnosis. Due to their buildup in the setting of vitamin B12 insufficiency, both intermediates will grow. (In folate insufficiency, just homocysteine will be raised).
The next step would be to look for the cause of a vitamin B12 insufficiency diagnosis to be made and confirmed. The patient's strict vegan diet is the most likely cause in this case. Even while electromyography and nerve conduction testing would show that neuropathy existed, they would not give the required details to identify the cause. Similarly, if other causes are ruled out, a computed tomography (CT) of the lumbosacral spine can be necessary. However, there are better courses of action than this when enough clinical data points to a vitamin shortage.
The best way to define the patient's folate and vitamin B12 levels is borderline. Therefore, there are better courses of action than administering a therapeutic dose of vitamin B12 without first determining what is causing the neurological symptoms. A bone marrow analysis would not be required now because the peripheral blood smear and complete blood count showed no further related cellular abnormalities. The cause is more likely to be discovered by less invasive tests (such as serum metabolite intermediates).
Based on radiographic findings, including the collapse of the subchondral bone in the afflicted joints and the presence of core erosions (as opposed to the marginal erosions of rheumatoid and psoriatic arthritis).
Erosive osteoarthritis (EOA) is indeed a subset of primary osteoarthritis (OA) that involves characteristic radiographic features. The diagnosis of erosive OA is primarily made based on the presence of central erosions and collapse of the subchondral bone in the affected joints. These radiographic findings help differentiate erosive OA from other forms of arthritis, such as rheumatoid arthritis (RA) and psoriatic arthritis (PsA), which typically exhibit marginal erosions.
An emergency department (ED) referral brings a 24-year-old patient in for a diagnosis of shortness of breath.
Reviewing the ED data revealed that the patient had minor respiratory distress, intermittent stridor, and frequent episodes of shortness of breath over the previous four months. At each presentation, oxygen saturation levels were normal. Intramuscular epinephrine and albuterol administered as empiric therapy did not affect the symptoms. The symptoms always went away on their own.
The patient's prior medical history is uneventful, and they are taking no drugs. The vital signs and physical exams are also typical right now. Which of the subsequent diagnoses is more likely?
The intermittent symptoms of this patient are most consistent with upper respiratory obstruction. The diagnosis most likely to be made is paradoxical vocal cord movements. Due to improper adduction of the vocal cords during inspiration in patients with paradoxical vocal cord motion, stridor, and respiratory discomfort ensue.
One sign of this potential diagnosis is a history of repeated visits to the ED for respiratory distress without any other obvious explanation. Exercise, among other things, can cause the symptoms to appear, and they usually go away independently. Although spirometry will show normal expiration and perhaps aberrant inspiratory function, it may be mistaken for asthma. The preferred diagnostic technique is laryngoscopy, which makes it possible to see the unusual cord movement in real-time.
After today's mechanical fall from ground level, a 71-year-old man with a right hip fracture is admitted to the hospital.
Surgery is scheduled for the evening and will be followed by orthopedic surgery. His prior medical history includes osteoarthritis, diabetes mellitus, hypertension, dyslipidemia, coronary artery disease, and hypertension. He uses insulin 70/30, metformin, lisinopril, atorvastatin, aspirin, metoprolol, and insulin. He used to be self-sufficient at home and go shopping by himself.
His nuclear myocardial perfusion imaging, performed six months previously for chronic atypical chest discomfort, revealed no evidence of ischemia. He expresses discomfort in his right hip.
Temperature is 36.8 degrees Celsius, blood pressure is 156/81 millimeters of mercury, pulse rate is 69 beats per minute, and respiration rate is 18 beats per minute.
Without radiation, hearing a grade II/VI early-peaking systolic murmur above the left sternal boundary is easiest. His right hip joint is painful, and his right lower extremity is rotated outward.
He can wiggle his toes and has good feeling in his right lower extremities.
The electrocardiogram displays a typical sinus rhythm with a few ventricular contractions that are premature.
The below laboratory workup is displayed. The best course of action is which of the following?
If surgery is put off for older patients with hip fractures, there is a higher risk of morbidity and death. Avoid using conservative therapy until the risks of surgery outweigh the advantages. According to data, having hip surgery within 48 hours of admission improves the prognosis. Delaying the procedure increases the risk of mortality and pressure sores even while the glucose is not under control. Instead of postponing surgery, it is preferable to manage the hyperglycemia (for instance, with an intravenous insulin drip).
A 32-year-old fit female patient comes in for a general checkup. She has no recognized medical conditions, either.
Every day, she runs 5 kilometers. Recently, she experienced dizziness while working out at the gym. She claims that she has never experienced something comparable before. She did say that it was a warm day with plenty of sunshine and that she had worked out a lot more than usual. She denies experiencing any palpitations, syncopal episodes, or chest discomfort.
One of her relatives, who is a medical student, quickly checked her vital signs. Her heart rate was constantly in the low 50s, which worried him. He recommended that she see a doctor for a checkup and additional investigation. Her EKG is shown. Which statement is accurate?
Sinus bradycardia can occur as a pathogenic reaction in several illnesses, but it also happens in healthy people as an adaptive response, especially in well-conditioned individuals or during sleeping. Sinus bradycardia is a common and typical finding in healthy children and adults, especially during sleep when rates may briefly dip as low as 30 beats per minute and pauses of up to two seconds are not unusual. Sinoatrial (SA) node dysfunction, sick sinus syndrome, an abrupt myocardial infarction, obstructive sleep apnea, and infections may all present with sinus bradycardia as their initial symptoms. The patient was generally healthy, but the clinical history is consistent with a vasovagal near-syncope.
Which statement about DDAVP (desmopressin) is accurate?
DDAVP, a vasopressin analog, can increase the ADH axis's activity and result in hyponatremia. Additionally, it has been demonstrated to promote endothelial cell release of von Willebrand factor. However, this medication might cause tachyphylaxis, and its effectiveness usually wears off after two or three consecutive doses. As a result, it cannot be administered again.
When von Willebrand factor attaches to glycoprotein 1, related to type IIB vWD, more platelets are cleared from the body. In individuals with type IIB vWD, DDAVP, which increases the release of von Willebrand factor, can result in thrombosis and severe thrombocytopenia and shouldn't be administered in this situation.