FREE Bachelor of Medicine & Bachelor of Surgery MCQ Questions and Answers
A dental operation is being performed on a 45-year-old male who had a prosthetic aortic valve replaced five years prior. Given its better absorption, which preventive antibiotics are advised?
Penicillin V and ampicillin are no longer used because oral amoxicillin has greater serum levels and absorption. Clindamycin is advised for individuals with penicillin allergies; other medications include cephalexin, ceftriaxone, azithromycin, and clarithromycin. Oral amoxicillin may be used when gut flora or enterococci are a possibility of exposure. Ampicillin may be administered if an IV regimen is necessary, and gentamicin may be added if the patient is at a high risk for endocarditis. Vancomycin is appropriate for people who are allergic to penicillin, with gentamicin given in high-risk cases. Only high-risk patients undergoing procedures with a high risk of bacteremia should use these parenteral regimens.
A 59-year-old man who has a slight fullness behind his right knee but no pain or restrictions in knee motion presents. He smokes 30 packs a year, consumes 1 to 2 beers socially each year, and takes hydrochlorothiazide to control his hypertension. He was examined because of a noticeable popliteal pulse, and duplex ultrasonography revealed a 3.4 cm popliteal aneurysm. His left lower extremity pulses are normal, as are the femoral and distal pulses on his right leg. The best course of action for management would be:
Popliteal aneurysms are managed according to their size and symptoms. Acute embolic limb ischemia, chronic limb ischemia with claudication, rest pain, or tissue loss, as well as compressive pain in the posterior fossa or radicular pain from neuronal compression, all of which should necessitate immediate surgical intervention, are symptoms that should be treated surgically. If the aneurysm is smaller than 2 cm in diameter, asymptomatic patients can be monitored regularly.
An 82-year-old woman presents with post-prandial dull abdomen pain that has been present for almost a year. She dropped 25 pounds in the previous three months as a result of avoiding oral intake due to worsening discomfort symptoms. Her symptoms have not improved after repeated normal upper endoscopies and long-term proton-pump inhibitor medication. She underwent a laparoscopic cholecystectomy six months earlier for several tiny gallstones, which were discovered during a right upper quadrant ultrasound. Four months ago, a colonoscopy revealed a solitary, fully excised pedunculated tubular adenoma. A CT scan was conducted, and it reveals no indication of cancer (see below). The patient is cachectic upon examination. Her abdomen is soft and not painful to the touch, and no lumps are visible. An analysis of the lab results reveals microcytic anemia and an albumin level of 2.4. The most effective course of treatment for this patient would be:
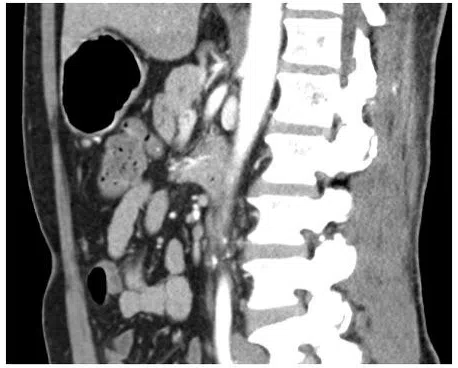
Due to its ambiguous appearance and ability to be confused with a variety of benign to malignant abdominal disorders, chronic mesenteric ischemia is frequently diagnosed later than it should be. The typical mesenteric ischemia presentation is an elderly patient with dull post-prandial pain (often referred to as "intestinal angina"), which over time results in severe food avoidance and frequently dramatic weight loss. In the CT angiography seen above, the superior mesenteric artery's origin is clearly narrowed. Cross-sectional imaging is not the most sensitive test for chronic mesenteric ischemia, and regardless of the results of the CT scan, the patient's symptoms should elicit additional diagnostic and therapeutic measures. A qualified vascular laboratory can use duplex ultrasonography to detect high-grade stenosis of the mesenteric vasculature in patients who have a suspicion of mesenteric ischemia. Mesenteric angiography with catheter guidance combined with angioplasty and stenting of the afflicted vessel is the gold standard for identifying and treating this disease. The use of appetite stimulants would not deal with the fundamental reason why the patient avoided food.
What pulmonary function test is the most effective at predicting postoperative performance when lobectomy is being considered?
Depending on other evaluable variables, most patients with a FEV1 above 60% expected will tolerate an anatomic lobectomy. Additional testing could be thought about if the FEV1 is less than 60% of what is indicated in an effort to determine the postoperative FEV1.
A 73-year-old man who has a history of atrial fibrillation and hypertension appears with mid-abdominal pain that started out of nowhere. A little while afterwards, I had a black, liquid bowel movement. There are no signs of peritonitis on an abdominal exam. The patient does, however, have leukocytosis. He is brought into the surgery room to be examined. The ascending colon, cecum, and distal small bowel appear dark and purple. What will management do next?
Bowel resection is done after revascularization. The objectives of surgical therapy for acute mesenteric ischemia are to resect any nonviable intestine and to (1) restore normal pulsatile flow to the SMA. Revascularization typically comes before resection. Depending on the precise underlying problem, several therapy modalities are used. The conventional course of treatment for SMA embolic disease is surgical embolectomy.
Which of the following statements about the lymphatic drainage of the lungs is true?
When analyzing left lower lobe lesions, it's critical to keep this in mind.
Which of the following statements about a tumor marker and the malignancy it is typically linked with is true?
It is true that CA 19-9, a serum marker for pancreatic cancer, is frequently employed.